The medicine is the message – Covid-19 vaccines have alerted the world to the power of RNA therapies | Briefing
MOLECULAR BIOLOGY is not a popularity contest. But if it were, it would be a partisan one. The evolutionary biologists would pledge their allegiance en masse to DNA. The sequences contained in its regular coils knit together the stories of almost all life on the planet. Pharmacologists, being of a more practical bent, would instead vote for proteins. Proteins are not about sequence, but about shape; their complex, irregular outlines, and the ways that they can change, allow them to do almost all of the biological work that gets done in cells. And it is thanks to the way that particular drug molecules fit into those shapes that almost all drugs have their effects.
Enjoy more audio and podcasts on iOS or Android.
There would be only a small following for ribonucleic acid (RNA), widely seen as a helpmeet molecule. It could be argued that the production of RNA is DNA’s main purpose; it is certainly true that the production of proteins would be nowhere without it. But it is a backstage operator, not a star; hewing wood and drawing water, hard working but hardly glamorous, appreciated only by devotees.
Or at least that was the case until vaccines made of RNA started giving protection against covid-19 to millions of people around the world every day. Now Cinderella has gone to the ball. Not only are RNA vaccines being considered for all sorts of other diseases, some of which have yielded to no other approach; other pharmaceutical uses of RNA look set to come into their own, as well. The way molecular biology is applied to medicine seems to be in the throes of revolution.
Incarnation incarnate
The great unifying truth of molecular biology, uncovered during the intellectual revolution which followed the discovery of DNA’s double-helix structure, is the way in which the worlds of shape and sequence are linked. The shape of a protein depends on the intricate way in which the chain of amino acids of which it consists is folded up. That depends in turn on the order in which amino acids of different types are strung together on that chain. And the order of the amino acids is a crucial part of the genetic information stored in the DNA sequences of the cell’s genome.
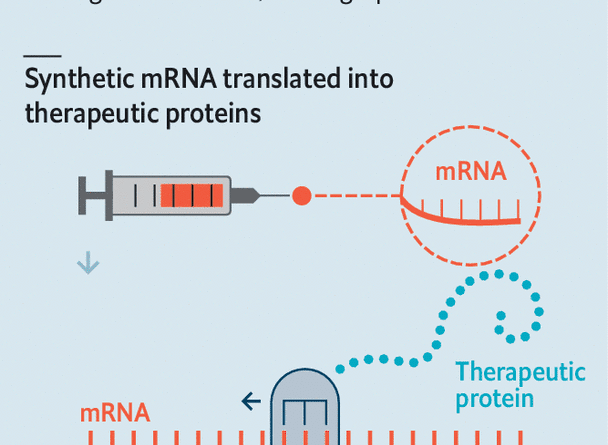
The transfer of information from the staid archival form it takes in the genome to its active physical instantiation in the machineries of the cell depends on RNA, a molecule in which both sequence and shape play crucial roles. The gene sequence is first copied from DNA to RNA; that RNA transcript is then edited to form a molecule called a messenger RNA, or mRNA (see diagram).

The end of the mRNA molecule is formatted into a distinctive shape which is recognised by ribosomes, complex pieces of machinery composed of dozens of proteins draped around another set of RNA molecules. With the help of yet more RNA molecules—little ones called tRNAs which stick to the mRNA sequence three letters at a time—the ribosome translates the genetic message into the protein it refers to by creating a chain of amino acids as it moves along the message.
This is the mechanism exploited by the RNA vaccines developed by BioNTech, a German biotechnology company based in Mainz, and Moderna, an American one from Cambridge, Massachusetts, against SARS-CoV-2, the virus which causes covid-19. The companies mass produce the RNA sequence describing the distinctive “spike” protein, which studs the outer membrane of the virus, formatted so as to look like a natural mRNA. These RNA molecules, wrapped in little fatty bubbles called liposomes are injected into patients, where the liposomes smuggle the mRNA into cells. Ribosomes pick up on the mRNA format and read the sequence, thus producing the spike protein. The immune system learns to recognise the spike which the vaccinated cells are producing and stores away the memory of how to do so. This allows it to mount a swift response if it later comes across the same protein on the surfaces of viral particles and infected cells.
This ability to get cells to churn out proteins for which their DNA contains no genes is, in itself, enough to open up swathes of new therapeutic territory. But it is not the whole story. Cells make vast amounts of RNA that does not describe proteins. Its ability to recognise specific genetic sequences makes it useful for all sorts of processes, including turning the translation of genes on and off. Its ability to fold itself into particular forms—hairpins, loops and the like—makes it good at interacting with proteins.
This alphabet soup of RNAs (see table) seems to function a bit like a computer’s operating system, mediating the relationship between the cell’s hardware and its software. Many of the details of how this works remain obscure. But some are understood well enough for a lot of brainpower and money to have been poured into attempts to hack the operating system for therapeutic purposes.

These abilities should enable drugmakers to head upstream from the proteins whose shapes they have long studied into the realms of sequence. Where previously they targeted proteins which were already present, now they can in principle target the processes which control which proteins get made in the first place, adding helpful new ones to the roster and crossing harmful old ones off. There are RNA-based drugs in clinical trials for the treatment of cancer, heart disease and numerous inherited disorders—as well as brain diseases such as Alzheimer’s and Parkinson’s.
Moreover, RNA’s mixture of sequence and shape means that in many of these areas the once-haphazard process of drug discovery, long dependent on matching the shape of small synthetic molecules to the crannies and crevices of the proteins they targeted, can itself be systematised. A sequence which recognises, or forms a part of, one gene can be switched out for a sequence tailored to another. When what an RNA drug does depends on its sequence, its target and action can be modified by the click of a mouse.
The medicine is the message
Both the firms with mRNA vaccines on sale had other vaccines in the pipeline before covid-19 struck. It is part of the appeal of the technology that they were able to turn on a sixpence and refocus their efforts on SARS-CoV-2 as soon as the sequence for its spike gene was released last January. Now they are both getting on with what they had planned beforehand. Moderna is looking at vaccines to fend off infection by cytomegalovirus (a herpes virus which causes neurological problems in newborns), three lung viruses which cause respiratory disease in young children and Zika, a mosquito-borne virus found mainly in the tropics. BioNTech is focusing more on developing vaccines, and other treatments, with which to treat a wide range of cancers.
Cancer cells tend to have peculiar constellations of proteins on their surfaces, including both normal ones that are overexpressed and, more intriguingly, mutant forms peculiar to the development of that tumour. Comparing the genes expressed in a patient’s healthy cells with those used by their tumour cells reveals which mutant proteins the cancers are producing; mRNAs for those proteins can then be incorporated into a vaccine.
Produced as a result of vaccination, the proteins can engender a vigorous immune response the cancer itself does not—part of being a successful tumour is deploying mechanisms that stop the immune system from coming to grips with you. According to Ozlem Tureci, BioNTech’s co-founder, the firm has 500 patients enrolled in clinical trials for cancer. Moderna is pursuing similar ideas.
BioNTech is also testing mRNA vaccines aimed at overexpressed but unmutated proteins. Moderna, meanwhile, is looking into vaccines that train the immune system to recognise proteins created by common mutations in KRAS, a gene implicated in about 20% of human cancers. CureVac, based in Tübingen, an mRNA firm which also has a SARS-CoV-2 vaccine in trials, is conducting trials of a vaccine for non-small-cell lung cancer.
Vaccination is not the only way that mRNA injection might fight viruses and tumours. The technique could also be used to get cells to produce therapeutic proteins that are currently administered through injection or infusion: interleukins and antibodies. Designer antibodies are a massive faff to make in industrial quantities; getting patients’ cells to take on the manufacturing duties instead would be a great step forward if it proved practical.
There are many other sorts of proteins which can be stimulated to therapeutic effect. A project on which Moderna is collaborating with AstraZeneca, a pharmaceutical giant, delivers the mRNA for a protein which encourages the regrowth of blood vessels. The idea is that the therapy, now in phase 2 clinical trials, could stimulate the growth of new cardiac blood vessels after heart attacks.
Getting the body to produce a protein it needs just for a short while—an antibody, say, or a growth factor—is one thing. But what about a protein that it needs on an everyday basis, but lacks the gene for? Such genetic diseases have always been the most obvious targets for gene therapy—treatments which add a missing gene to a patient’s cells, or repair a broken one, thus allowing them to make a protein they have hitherto lacked. But at least some such conditions might instead be treated with mRNA. Inserting a gene might be more elegant—but getting it in the right place and regulated in the right way is challenging. If mRNA treatments get the job done, they might offer a nice alternative.
There are thus mRNA treatments being studied for phenylketonuria, a metabolic disorder which requires sufferers to restrict their diets for their entire lives; glycogen-storage disease, which enlarges the liver and kidneys and stunts children’s growth; and propionic and methylmalonic acidemias, two illnesses in which the body cannot properly break down proteins and fats. All are conditions that gene therapists are looking at, too.
That BioNTech, Curevac, Moderna and some others now have all these projects on the go is largely down to the fact that they have spent many years developing the basics of their platforms. Many hurdles had to be crossed before they could get cells to accept and act on messages from beyond; the RNA had to be subtly toughened up so that it would not itself fall prey to the immune system or get dismantled inside cells; the right lipids had to be found for delivery, sometimes tailored to particular tissues like those of the liver or lymph nodes. The potential inherent in the idea meant that their work was not completely ignored; in 2018 Moderna’s IPO valued the company at $7.5bn, a record for the biotech sector. But biotechnology has a long history of proving biology to be messier and more contrary than those seeking to exploit its loopholes expect.
Stop making sense
Scepticism was also warranted, it seemed, by the fact that messing around with RNA had been through bursts of popularity before. One of the very oldest companies in the field, Ionis Pharmaceutials (known as Isis until that name was appropriated by a would-be caliphate) was founded in 1989. Its intention, then and now, was not to make use of mRNA, but to hobble it.
The sequence of an mRNA molecule carries the same information as can be found in the gene which served as its template; but thanks to the way RNA is made it carries it in a complementary way. Where the DNA has a letter called C for cytosine, the RNA will have G for guanine; where the RNA has a C the DNA will have a G, and so on. Complementary strands stick together; that is what keeps DNA molecules paired up in double helices. If you introduce an mRNA to a molecule with a complementary sequence the two will stick together, too, rendering the mRNA useless (see bottom deck of diagram above).
Again, getting the neat idea to work in ways that helped proved hard. It took Ionis a quarter century to start getting its “antisense” drugs to market on a regular basis. It now has three: nusinersen, approved in America in 2016 and Europe in 2017 for use against childhood spinal muscular atrophy, a muscle-wasting illness; inotersen, approved in 2018 for hereditary transthyretin-mediated amyloidosis (hATTR), which damages the peripheral nervous system; and volanesorsen, approved in Europe in 2019, which lowers levels of triglyceride fats in the blood of people with a metabolic error that makes them far too high.
Ionis currently has a further 37 antisense molecules in clinical trials for conditions including Huntington’s disease (a study being carried out in collaboration with Roche, a large Swiss pharma company); amyotrophic lateral sclerosis, Alzheimer’s disease and Parkinson’s disease (in collaborations with Biogen, a specialist in treatments for neurological disease); beta thalassaemia, a blood disorder similar to sickle-cell anaemia; and cystic fibrosis.
The firm is also developing, in collaboration with Novartis, another Swiss company, a way of reducing levels of lipoprotein(a), a particularly damaging form of low-density-lipoprotein (LDL) cholesterol. Lipoprotein(a) levels are untreatable with existing medicines; Pelacarsen, as the drug is known, is in phase 3 clinical trials to see if it can change that.
Unlike molecules of mRNA, which can tolerate only a small amount of chemical tinkering before becoming ribosome-unfriendly, antisense molecules can be tweaked quite a bit, and thus made long-lasting. Ionis’s researchers have worked out how to stabilise them so that they will hang around inside cells for months. This is important because most of Ionis’s targets are chronic diseases that require continuous treatment. The fewer injections per year the better.
While biotech companies were beavering away at antisense molecules in the 1990s, researchers elsewhere discovered that nature had a similar technology of its own: gene silencing, a process guided by small interfering RNAs (siRNAs). The early 2000s saw a gene-silencing biotech boom led by Alnylam, founded in Cambridge, Massachusetts in 2002, and Sirna Therapeutics, which got going in San Francisco the following year.
Established pharma companies, including Abbott, Merck, Novartis, Pfizer, Roche and Takeda, waded in, too, with Merck buying Sirna for more than $1bn in 2006. For almost a decade, attention and money were showered on the field. But though there were many promising leads, they failed to turn into drugs. By the early 2010s it seemed that the party was over.
Nonlinear, nonvisual and inclusive
Alnylam, though, kept dancing. In 2014 it bought what was left of Sirna from Merck for a knock-down price. It launched its first product, patisiran, a treatment for hATTR, in 2018. It now has two others, givosiran and lumasiran, which also address rare genetic disorders.
A fourth substance developed using its technology has broader appeal. This is inclisiran, developed to treat an inherited disorder that pushes the concentration of LDL cholesterol in the blood to dangerous levels; around 30m people worldwide suffer from it. A firm called the Medicines Company licensed Inclisiran from Alnylam to bring it to market. With approval looking likely (it was given in Europe late last year) Novartis bought the Medicines Company for $9.7bn in January 2020.
According to Akshay Vaishnaw, Alnylam’s head of R&D, the firm has another 14 siRNA drugs in clinical trials. These including potential treatments for haemophilia, hepatitis B and recurrent kidney stones. Arrowhead Pharmaceuticals, of Pasadena, California, has eight potential siRNA drugs in trials, including one directed at cystic fibrosis. Dicerna Pharmaceuticals, of Lexington, Massachusetts, has three.
These siRNAs work by straddling the worlds of shape and sequence. Their shape fits them into a group of proteins called an RNA-induced silencing complex (RISC). But a bit of the siRNA is left sticking out of this complex; this tail contains a sequence complimentary to that of the RNA to be silenced. When siRNA and mRNA meet, the proteins in the RISC chop the messenger to pieces. (A conceptually similar mechanism for the RNA-guided protein-executed chopping up of genes found in bacteria is the basis of the CRISPR tools now revolutionising gene editing.)
In plants and invertebrates the natural function of the siRNA mechanism is clear: cutting up mRNAs associated with viruses. They do not seem to serve that function in vertebrates, and no one is quite sure what they do instead. But that does not stop them from looking like promising drugs.

So do another set of RNAs associated with RISCs: micro-RNAs, which use their complementary sequences not to destroy mRNAs but to regulate them. The human genome seems to contain about 2,600 of these miRNAs, and they are thought to be involved in regulating the rate at which about 60% of the genes describing proteins get transcribed. Several look like promising therapeutic targets.
Since the active bit of an miRNA is a single-stranded sequence-specific tail, the obvious way to target them is with antisense. Regulus Pharmaceuticals, a firm that started life as a collaboration between Ionis and Alnylam, is trying to develop antisense molecules aimed at miRNA-21 to treat two kidney-related genetic conditions in which that miRNA plays a role. When you start targeting miRNAs, though, things get positively baroque. Santaris Pharma, a Danish firm, has developed Miravirsen, an antisense suppressor for miRNA-122 which the hepatitis C virus uses for its own unhelpful ends. The drug has now been taken on by Roche.
The innovation continues. MiNA Therapeutics, a startup in London, is working on the potential of saRNAs, which activate genes which otherwise stay silent. Others are investigating systems for “self-amplifying” mRNA drugs. These mRNAs would inveigle a cell’s ribosomes into producing not just the protein that was meant to be delivered, but also a second protein, called RNA-replicase, which would make more of the mRNA, thus leading to even more protein being expressed. There is surely further cleverness to come.
Could be so exciting

Even if only a fraction of these possibilities pan out it looks certain that, in popularity contests to come as in stockmarkets today (see chart), more people will be plumping for RNA. Their support will be welcomed by the small band of biologists with an interest in the very earliest history of life that has long formed the discerning core of the molecule’s following. Life needs both a way of doing things in the now—catalysing the reactions on which its metabolism depends—and of passing information into the future. Of the molecules known today only RNA, in its shape-and-sequence versatility, can do both those things, dealing with the needs of the everyday at the same time as encoding instructions for its own reproduction in the form of a legible sequence. This suggests to many that early life spent some time in an “RNA world” before the division of labour allocated doing things to the proteins and storing data to DNA, reducing RNA to a supporting role in the world it had created.
The application of RNA has met many obstacles over past decades, and the fact that it has proved itself in vaccines does not mean it will not meet more in the future. But it does seem that medicine now has a way to target drugs not just at proteins, but at the processes that make them, and that opens up new realms of possibility. The next RNA world awaits. ■
Dig deeper
All our stories relating to the pandemic and the vaccines can be found on our coronavirus hub. You can also listen to The Jab, our new podcast on the race between injections and infections, and find trackers showing the global roll-out of vaccines, excess deaths by country and the virus’s spread across Europe and America.
This article appeared in the Briefing section of the print edition under the headline « A new phaRNAcopoeia »