In Its First 100 Days, The Biden Administration Must Restore The Soul Of Medicaid
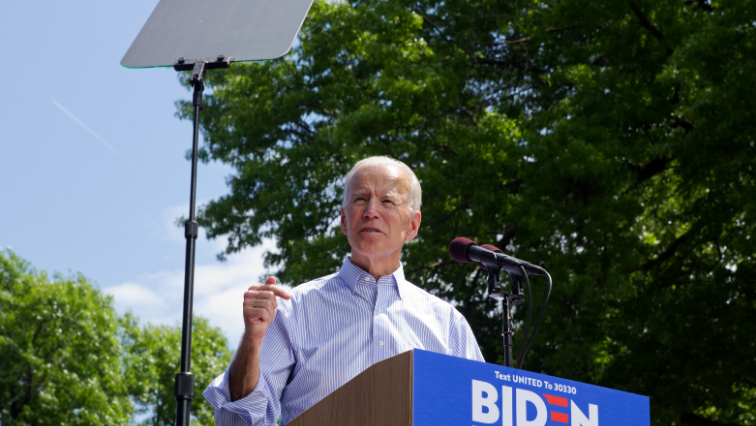
President-elect Joe Biden will enter office facing exceedingly important first days. Immediately, he must address ongoing health and economic emergencies. A top priority should be steadying and rebuilding Medicaid, the health care safety-net program that covers nearly one-quarter of the population.
Medicaid expansion under the Affordable Care Act (ACA) has been adopted in 38 states and the District of Columbia and has been extensively studied since 2014. Evidence shows that expansion has increased access to care for those who are unlikely to be offered employer-sponsored insurance and who often cannot afford it (such as low-wage and part-time workers), as well as historically underserved populations, such as people of color. From 2013 to 2017, Medicaid expansion narrowed the disparity in insurance coverage between Black and White populations from 11.0 to 5.3 percentage points, and between Hispanic and non-Hispanic White populations from 25.4 to 16.6 percentage points.
The Trump administration weakened many features of Medicaid that make it uniquely reliable for low-income people and for states, especially in times of crisis, such as continuous eligibility, comprehensive benefits, limitations on out-of-pocket payments, and guaranteed federal matching funds to states. From day one, the administration demonstrated a desire to eradicate the ACA or to diminish its reach if Congress did not repeal it, introducing novel policies intended to weaken Medicaid’s unique protections for low-income populations with a focus on undercutting enrollment of the expansion population.
Some of the highest-profile Medicaid policies implemented by the Department of Health and Human Services (HHS) in the past four years are patently unlawful, such as demonstration projects that allow work requirements and block granting of federal Medicaid funds. Other policies, such as reduced coverage of non-emergency medical transportation, limitations on retroactive eligibility, and frequent eligibility redeterminations, thwart the program’s purpose by weakening coverage and access to care. These policies have been implemented through executive branch decisions, so the incoming administration can quickly begin the work of unwinding them without waiting for Congress. The Biden administration has no time to lose, as the US Supreme Court recently granted a petition by Arkansas and New Hampshire to have their Medicaid work requirements declared legal. Stabilizing Medicaid will go a long way toward improving the circumstances of disadvantaged populations who are hit hardest by COVID-19 in the near term and beyond. To this end, the game plan for the first 100 days should prioritize four critical changes:
Rescind Work Requirements
To begin, the new HHS secretary should rescind the 2018 State Medicaid Director Letter (SMD) titled “Opportunities to Promote Work and Community Engagement Among Medicaid Beneficiaries,” which was issued after Congress failed to repeal the ACA in 2017 and allows states to require work or other “community engagement” (such as job training or volunteer programs) as a condition of Medicaid eligibility for the first time in the program’s history. Fifteen states have received HHS approval for demonstration projects that include work requirements, but three states voluntarily withdrew their demonstrations (Kentucky, Maine, and Virginia), and four states have had their 1115 waivers stayed by federal courts (Arkansas, Kentucky, Michigan, and New Hampshire). Seven more states have waivers pending at HHS that include work requirements. Some of the states that have implemented work requirements, such as Arkansas, had expanded Medicaid and focused work requirements on the expansion population, but other states, such as South Carolina, had work requirements approved without Medicaid expansion. Yet, unlike work requirements in the Supplemental Nutrition Assistance Program and Temporary Assistance for Needy Families, Medicaid work requirements are not authorized by federal law. And, despite HHS’s assertions to advance the policy, these requirements are contrary to the program’s purpose. In the limited time they have been implemented, work requirements led to substantial disenrollment from Medicaid but not more employment in jobs with health benefits.
Once the 2018 policy is revoked, HHS should reject any demonstration waiver applications seeking to implement work requirements. What to do with waivers already approved is less straightforward. When HHS approves state waiver applications, it reserves authority to amend or withdraw approval (or eliminate funding authorization) if it determines that a waiver or any part of it would no longer be in the public interest or promote Medicaid’s objectives. The Biden administration could withdraw approval of entire waivers or certain elements such as work requirements, but states can appeal such decisions. Because the approved 1115 demonstrations contain much more than just work requirements, efforts to eliminate them are particularly complicated. Therefore, another option would be for HHS to invite states to renegotiate the waivers to remove work requirements while keeping other provisions intact. Of course, states could follow the lead of Kentucky, Maine, and Virginia and simply terminate waivers granted by the Trump administration. This would save time and money as well as undue confusion for Medicaid beneficiaries.
Whether or not HHS seeks to withdraw or renegotiate the approved work requirement waivers, their fate ultimately may rest with federal courts. In a somewhat surprising move, the US Supreme Court granted Arkansas and Trump administration petitions for certiorari on December 4 in Arkansas v. Gresham and Azar v. Gresham. The Court will hear the case in early 2021. Biden’s new solicitor general should withdraw federal support for the claim by Arkansas and New Hampshire that their 1115 work requirement waivers are lawful. Rescinding the 2018 SMD letter and withdrawing from defense of the waivers in court would likely render the case moot. However, other litigation could arise from remaining states’ 1115 waivers.
So far, federal judges have uniformly struck down work requirement waivers as “arbitrary and capricious,” coming close to ruling that work requirements contradict the purpose of Medicaid but not clearly holding that they are illegal. Rather, federal courts have held that the comment and approval processes were deeply flawed, an issue that has arisen for the Trump administration in other cases. Due to these judicial decisions and the ongoing COVID-19 pandemic, no state currently is implementing work requirements. But allowing the work requirement waivers to linger places low-income populations at risk; the short-lived implementation of the policy in Arkansas led to disenrollment of 18,000 beneficiaries.
Revoke The Block Grant Initiative
The second policy that should be revoked is the Healthy Adult Opportunity (HAO) initiative. In early 2020, the Centers for Medicare and Medicaid Services issued an SMD letter inviting state applications for Section 1115 waivers to convert Medicaid funding for certain populations to block grants or limits on per capita spending, offering states less federal oversight in exchange for limited funding (while also continuing to encourage work requirements for the expansion population). However, Section 1115 does not give HHS authority to waive Section 1903 of the Social Security Act, which governs the provision of federal Medicaid matching funds to states. The block grant policy therefore is unlawful and would likely face a fate similar to that of the work requirement waivers; however, no court has had a chance to rule on the HAO initiative.
So far, just two states have sought to participate in the HAO initiative. Oklahoma submitted a waiver application but later withdrew it due to a successful ballot initiative to expand Medicaid. Tennessee submitted a block grant waiver application before the HAO initiative was launched. Because HHS has not yet approved either application (see update below), revoking the HAO initiative would be relatively straightforward. HHS could formally reconsider the policy, interpret it to be unlawful, and rescind the SMD letter that announced it. Such action would preclude the submission of any additional HAO waiver applications. At the very least, the new HHS secretary should clarify as a matter of policy that HAO waiver proposals are unwelcome. Such action is especially important given Medicaid’s role as a social safety net during the pandemic; its unlimited federal matching funds are supporting the program at the very moment states are losing revenue while facing increased enrollment.
Reverse Policies That Cut Benefits
Another category of problematic 1115 waivers are those allowing increased Medicaid cost sharing and limits on benefits and coverage. Some of these policies began during the Obama administration as part of negotiations with states to expand Medicaid eligibility under the ACA. They should not be continued by the Biden administration. For example, by law Medicaid typically covers services for the three months prior to enrollment if a new beneficiary would have been eligible during that time period, known as retroactive eligibility. This is the kind of special protection for low-income populations that is unique to Medicaid. Over the past several years, HHS has approved 1115 waivers allowing states to eliminate retroactive eligibility. Waivers also have allowed states to charge premiums coupled with lockouts—which permit states to drop beneficiaries from coverage for nonpayment—and to require more frequent eligibility redeterminations. The increased administrative burden on enrollees and the heightened risk of paperwork errors associated with frequent redeterminations often lead to disenrollment. Such provisions not only flout evidence that paperwork and out-of-pocket costs are barriers to enrollment, but they also undercut Medicaid’s core protections for low-income populations.
Restore Access To Planned Parenthood Services
Lastly, HHS under the Trump administration emboldened states to violate Medicaid’s free-choice-of-provider requirement by allowing them to eliminate Planned Parenthood as a qualified provider for payment purposes. This policy has been rejected by most federal appellate courts. However, the Fifth Circuit recently held in Planned Parenthood v. Kaufmann that beneficiaries do not have standing to challenge state decisions to eliminate providers from Medicaid. As a result, Texas is able to prohibit Medicaid payments to Planned Parenthood, at least while litigation continues. The prohibition on payments to Planned Parenthood significantly restricts low-income patients’ access to mammograms, Pap smears, and other preventive care, such as screening for sexually transmitted infections. The Biden administration should reinstate the Obama-era guidance instructing states that Medicaid’s free-choice-of-provider policy bars the exclusion of Planned Parenthood.
Moving Forward
To effectively confront the health and economic crises facing the nation now and into the future, maintaining a robust Medicaid program is essential. Medicaid expansion functions as a tool to protect individual and public health—addressing social determinants, diminishing entrenched disparities, and improving coverage and access to care for vulnerable communities—and to stabilize state budgets. Medicaid expansion remains the law of the land, despite repeated efforts by the Trump administration to undermine the program, along with the ACA generally. Incoming HHS Secretary Xavier Becerra must quickly take action to strengthen Medicaid. Prioritizing the program would build on his work to support the ACA while serving as attorney general of California. No other public program has the reach and power to affect population health that Medicaid does, particularly for historically poor and oppressed communities. Time is of the essence to rebuild and preserve Medicaid as a source of hope and help, not one of frustration and fear.
Update
On January 8, 2021, more than a year after its submission, CMS approved the Tennessee block grant waiver amendment application for 10 years. The incoming Biden administration has several avenues through which it could address this last-minute approval, which include withdrawing the HAO policy, delaying implementation, and revoking approval of the waiver. An additional complicating factor could be a letter that CMS sent recently to state Medicaid directors, asking them to sign new waiver terms designed to slow revocation or renegotiation of approved waivers. Undoubtedly, patients, community organizations, and/or health care systems will challenge the legality of the waiver in federal court, as section 1115, the statutory authority for demonstration projects, does not provide the Secretary authority to waive section 1903 of the Medicaid Act governing the federal matching payments to states.